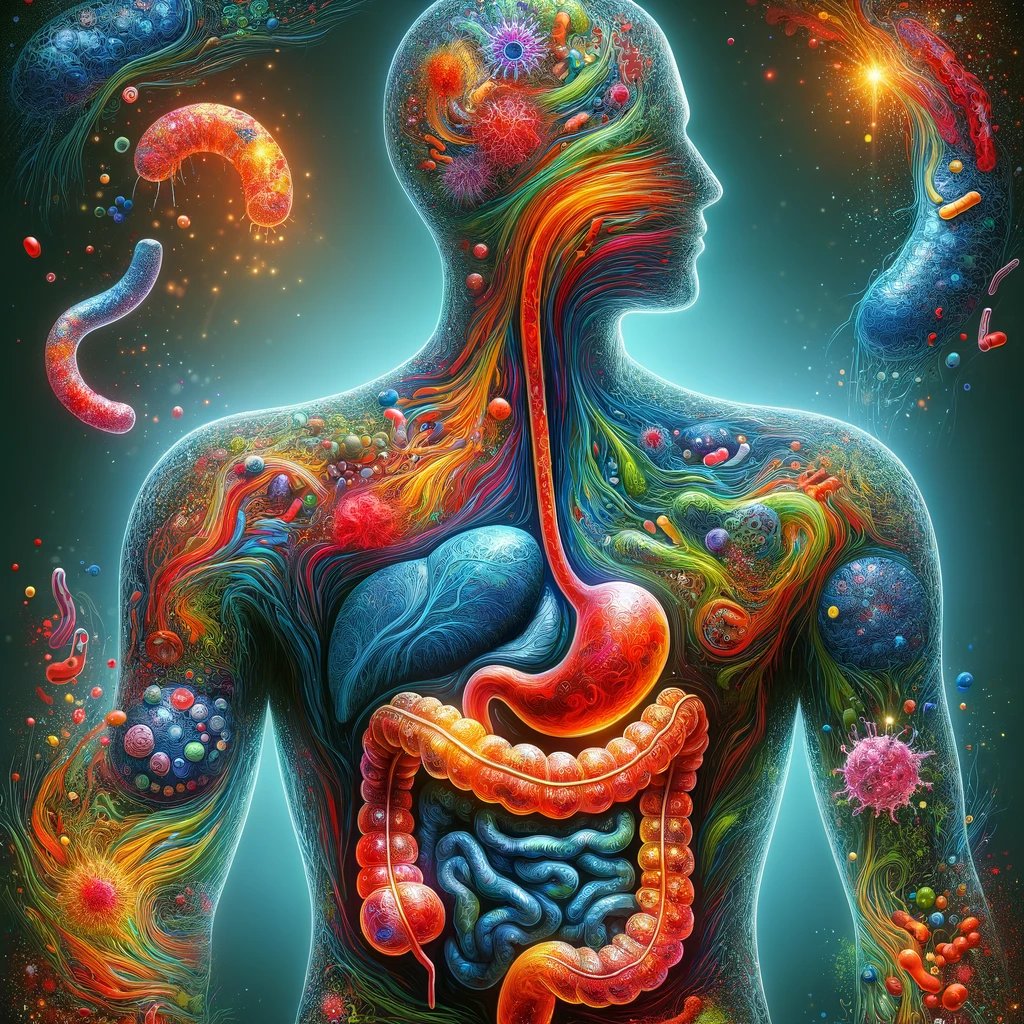
In recent years, the gut microbiome has emerged as a key player in our overall health, influencing everything from digestion to mood regulation. Among its roles, the relationship between the gut microbiome and gastrointestinal disorders such as Irritable Bowel Syndrome (IBS) and Inflammatory Bowel Disease (IBD) has gained particular attention. This blog post delves into the complexities of this relationship, exploring how imbalances in gut bacteria can contribute to the development and symptoms of these conditions and what management strategies might look like.
The Gut Microbiome and Irritable Bowel Syndrome (IBS)
IBS is a common disorder characterized by symptoms like abdominal pain, discomfort, and altered bowel habits. Recent research points to an imbalance in the gut microbiome, or microbial dysbiosis, as a contributing factor to the syndrome. Patients with IBS often exhibit an increase in certain harmful bacteria, such as Firmicutes, and a decrease in beneficial ones like Bifidobacterium. This imbalance can lead to low-grade intestinal inflammation, a hallmark of IBS. Interestingly, some bacteria, like Faecalibacterium prausnitzii, have shown promise in reducing IBS symptoms by maintaining gut mucosal health and integrity.
Potential Protective Bacteria and Probiotics in IBS
While the gut microbiome’s role in IBS is complex, certain bacterial groups have been identified as potentially protective. The uncultured Clostridiales and Bifidobacterium, in particular, have been associated with alleviating IBS symptoms. Probiotic interventions containing Bifidobacterium have demonstrated effectiveness in reducing IBS symptoms, highlighting the potential of targeting specific bacterial groups as a therapeutic approach.
Dietary Management of IBS: The Low FODMAP Diet
Diet plays a crucial role in managing IBS symptoms, with the low FODMAP (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) diet showing promise in clinical studies. This diet involves restricting certain carbohydrates that can aggravate symptoms. However, its efficacy can vary among individuals, potentially due to differences in gut microbiome composition. This has led to growing interest in using the gut microbiome to predict who might benefit most from a low FODMAP diet.
Inflammatory Bowel Disease (IBD): A Closer Look
IBD, which includes conditions like Crohn’s disease and ulcerative colitis, is characterized by chronic inflammation of the gastrointestinal tract. Similar to IBS, microbial dysbiosis is implicated in IBD, with patients typically showing a decrease in microbial diversity and stability. Notably, a reduction in beneficial Firmicutes and an increase in harmful Proteobacteria are common findings. These shifts in the gut microbiome can contribute to the inflammation and ulceration seen in IBD.
The Therapeutic Potential of Butyrate in IBD
Among the strategies to address microbial dysbiosis in IBD, the supplementation of butyrate-producing bacteria has shown promise. Butyrate plays a vital role in maintaining gut health by serving as an energy source for colonocytes, enhancing barrier integrity, and reducing inflammation. Probiotic interventions aimed at increasing butyrate production in the gut have been explored as potential treatments, offering a glimpse of hope for restoring gut homeostasis in IBD patients.
The Future of Gut Health Management
The exploration of the gut microbiome’s role in gastrointestinal disorders like IBS and IBD underscores the intricate connections between our diet, microbiome, and health. As research progresses, personalized dietary interventions and probiotic treatments targeting specific bacterial imbalances hold great promise for managing these conditions. By understanding and harnessing the power of the gut microbiome, we move closer to developing more effective strategies for promoting gut health and alleviating the symptoms of gut inflammation and bowel disorders.